A family struggles with a history of diabetes and its future
When I was 7, my dad gave up smoking. He traded in the
nicotine-laced cigarettes for hard candy that he carried in his
pocket everywhere he went. A younger cousin, who was about 3 years
old at the time, took to calling my dad the lifesaver man.
A family struggles with a history of diabetes and its future
When I was 7, my dad gave up smoking. He traded in the nicotine-laced cigarettes for hard candy that he carried in his pocket everywhere he went. A younger cousin, who was about 3 years old at the time, took to calling my dad the lifesaver man.
Through the years, my dad always had some sort of sweets in his pocket. For a while it was Mentos – the fruit-flavored ones that are packed with sugar. Then Necco wafers. He had them in his lunch pail, his pants pockets and kept a stash in his bedside drawer. He’d chew a few before going to sleep at night and as soon as he woke up, before brushing his teeth, he’d pop in a few more.
As far as vices go, my family thought the penchant for sweets was mild. Sure the bits of wrappers left around were annoying and sometimes we got annoyed with the constant crack of Necco wafers in his mouth, but it sure beat the smell of cigarette smoke.
Last December, my dad was diagnosed with type 2 diabetes and all those years of chewing on sugar-filled sweets seemed a lot less harmless than they had. He had had a thorough check-up less than nine months before with no worries except for a minor case of acid reflux and high blood pressure, for which he had long been on medication. The recent visit had only been because he needed to see the doctor before getting a refill on his blood pressure pills.
“I was surprised,” my mother said. “I didn’t really think he would get it because they say it’s mostly overweight people.”
My dad has always been the thin one in our family and among his siblings. He is short, maybe 5-foot-4, and sleight with skinny legs and muscular arms. He has a pot belly that has made an appearance in the last decade, but few men over 50 maintain a flat stomach.
Receiving a common diagnosis
Each year 1.5 million new cases of diabetes are diagnosed, according to the Centers for Disease Control and Prevention. In 2005, 20.8 million Americans – or 7 percent of the population – had been diagnosed with diabetes.
“We are seeing more and more diabetes in this community,” said Jennifer Bange, a dietician at Hazel Hawkins Memorial Hospital. “And there is definitely a genetic component.”
Last year, my father was one of many. His youngest sister had already been diagnosed. Another sister exercises voraciously to avoid it. They all knew they were at higher risk for the disease because they are Mexican-American and their mother had it. After years of taking medication to control her blood sugar levels, my grandmother had to go on dialysis for kidney failure and a few months later, when I was 15, she died.
“I knew it had to do with high sugar in the blood system,” my dad said when I asked him about his diagnosis recently. “I didn’t know how it affected me, but it does affect you a lot. I thought about it, but I thought it would happen later because [my mother] got it when she was older.”
My dad turns 59 on Sunday, July 1.
Caucasians have the lowest incidence of diabetes, though the numbers of people diagnosed with the disease is increasing across the board. Mexican-Americans are 1.7 times more likely to get diabetes than non-Hispanic whites. African-Americans are 1.8 times more likely to get it than non-Hispanic whites.
The incidence is off the charts in pockets of Native American and Alaskan Native populations. In southern Arizona, as many as 28 percent of the population of Natives have the illness. Asian Americans and Pacific Islanders also have a higher rate.
When my dad was first diagnosed, I thought of all the worst things that could happen – the kidney failure, the blindness, and amputations. I remembered what happened with my grandmother – and a part of me wonders if this is something that is already predestined for me. Is the disease already coursing through my blood and is it just a matter of time before I am diagnosed?
“A strong family history and serious side effects can lead to a lot of fear,” said Michaele Johnson, a registered nurse and certified diabetic educator at Hazel Hawkins.
Hispanics have a further complication in that many of them are insulin-resistant so drugs to treat diabetes that didn’t cause damage to the body were rare.
“Those with type 2 [diabates] are really blessed – not to have the disease – but to have it now in the last ten years,” Johnson said. “They can start on meds and live for many years. New drugs help them maintain better control.”
Wading through the misinformation
At first, my family was left without much guidance. My father’s doctor spent 15 minutes with him during his diagnosis and then told him to make an appointment with a health educator at the local hospital. There was no mention of what foods to avoid and what foods to eat. There was no talk about how common the dreaded complications are. The doctor didn’t even encourage him to add a little activity to his daily routine.
“I was worried about how to control it. I didn’t know what kind of food I had to eat and things like that,” my dad said. “You can eat almost everything. You can eat the same, but basically in small proportions or limited on certain kinds of food.”
Bange suggests a diet based on the food pyramid for most of the diabetic patients she works with.
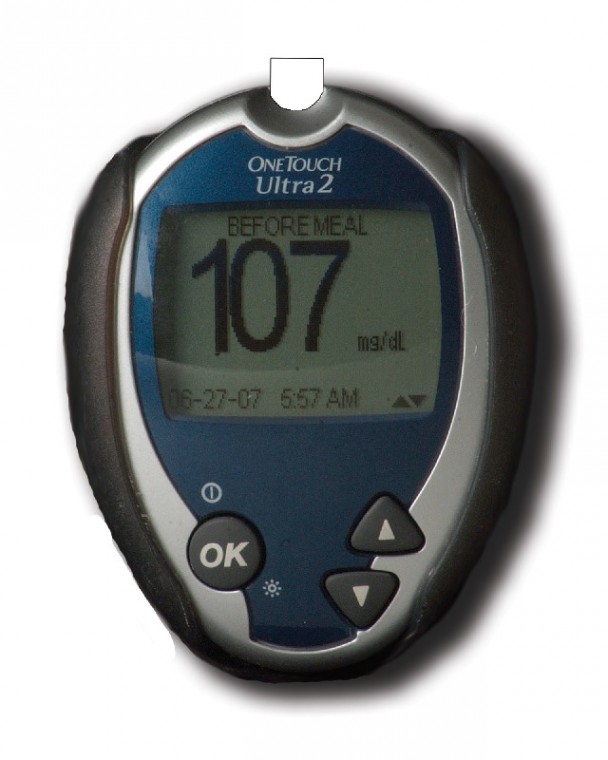
For most people, two hours after eating, their blood glucose level should be below 140. In a diabetic, the blood glucose level is more than 200 and for a person who is pre-diabetic, their level is between 140 and 199. The goal with diabetics is to avoid foods that spike the glucose level and to keep it steady. Eating carbs throughout the day in small proportions can help, Bange said, rather than eating a larger serving of carbs once a day.
“The new thing about the diabetic diet is that diabetics can eat a wide variety of foods,” Bange said. “It’s just a matter of controlling the amount of carbohydrates.”
Still it isn’t always easy to navigate through all the information.
“There are so many mixed messages,” Bange said. “I have patients come in and tell me, ‘I didn’t think I could eat carrots because carrots have sugar.’ When you look at a cup of raw carrots it has a lot less sugar than, say, a cup of fruit juice.”
My parents struggled with the same misinformation when my father was first diagnosed.
“I think the most frustrating thing was the misconceptions because we hear, ‘oh you can’t have fruit or you can’t have that,'” my mother said. “Everything everyone hears might not be accurate.”
Even from those who were being treated for diabetes, the information was contradictory. One person told us that my dad should never have more than 14 grams of carbohydrates in any meal. The first week we did the grocery shopping, my mom and I frantically looked at nutritional information. Even the healthiest cereals had 20 grams of carbs per serving and anything but the fattiest foods seemed to be over the 14 gram limit.
It wasn’t until my mom and dad attended their first diabetes class that they learned that about 50 percent of daily calories should come from carbohydrates. When an item has more than 5 grams of dietary fiber, as some cereals do, it can be subtracted off the total carbs. Suddenly the task of keeping my dad healthy seemed less daunting.
Taking control of our health
While medications have improved, Johnson expressed frustration that the incidence of diabetes continues to rise.
“It’s related to food choices,” she said. “We are so computer minded. We sit at desks and tables all day.”
The hospital received a grant last year to change thoughts about healthy eating and physical activity in the most pliable population in the community – children. Johnson and others went to schools and met with kindergartners and their parents. Their program talked about healthy food choices and easy ways to exercise, such as yoga, which requires little equipment and can be done nearly anywhere. In one program, Johnson showed how many spoonfuls of sugar were in sweet drinks such as Capri-Sun or nectar juices. The audience was shocked at the amount of sugar in drinks that were labeled “natural.”
One of the benefits of my dad’s diagnosis is that it has served as a wake-up call for me. Researchers agree that moderate weight loss and exercise can prevent or delay type 2 diabetes among adults at a high risk, according to the CDC.
“If you have a healthy lifestyle even with a predisposition to diabetes, you can get into your 70s before being diagnosed,” Johnson said.
Even those who have been diagnosed with pre-diabetes – a condition in which fasting glucose levels are high but not to diabetic levels – can still reverse the course of their medical destiny.
“There was a big study done – a diabetes control trial,” Bange said. “Basically what that study showed is that the tighter the blood sugar control, the less risk of developing long-term complications of diabetes. It is consistently running high blood levels that does damage in the body and it affects so many different systems in the body.”
The best prevention for diabetes or control for those already diagnosed is to maintain a healthy weight and exercise, Bange said.
In more recent months, I have started wearing a pedometer every day of the week. It feels a little dorky sometimes, but it reminds me that I need to be active. I take off for 30-40 minutes during my work day and walk. I don’t have a destination or purpose except to shave off a few thousand steps from my daily goal. I don’t always get there, but I know I am moving in the right direction.
As for my dad, we still need to remind him to eat when he gets busy around the house or to pack extra food if he is going to be working overtime so that his blood sugar stays level. We try to get him active – an easy thing to do since we got a dog a couple months ago who needs regular walks.
One thing that hasn’t changed is that he’s still got hard candy in his pockets everywhere he goes – it’s just sugar-free now.
Resources:
For more information on diabetes prevention or living with diabetes, visit the American Diabetes Association Web site at www.diabetes.org or call 1-800-DIABETES (1-800-342-2383).
Hazel Hawkins Hospital hosts a diabetes support group the third Monday of each month at 7 p.m. in the Gil Gallery. Meetings are on hiatus for the summer and will resume in September.
Complications from diabetes:
The many disorders associated with diabetes make it important for those who are diagnosed to keep their blood sugar under control and see a doctor regularly to detect early signs of other illnesses.
Below are the most common complications from diabetes.
Heart disease and stroke – People with diabetes have an increased risk of heart attack, stroke, and complications related to poor circulation. Two out of three people with diabetes die of heart disease or stroke.
Kidney disease – Diabetes can damage the kidneys, which not only can cause them to fail, but can also make them lose their ability to filter out waste products.
Eye complications – Diabetes can cause eye problems and may lead to blindness. People with diabetes do have a higher risk of blindness than people without diabetes. Early detection and treatment of eye problems can save your sight.
Diabetic neuropathy and nerve damage – One of the most common complications of diabetes is diabetic neuropathy. Neuropathy means damage to the nerves that run throughout the body, connecting the spinal cord to muscles, skin, blood vessels, and other organs.
Foot complications – People with diabetes can develop many different foot problems. Foot problems most often happen when there is nerve damage in the feet or when blood flow is poor and can lead to amputations if not treated. Learn how to protect your feet by following some basic guidelines.
Skin complications – As many as one-third of people with diabetes will have a skin disorder caused or affected by diabetes at some time in their lives. In fact, such problems are sometimes the first sign that a person has diabetes. Luckily, most skin conditions can be prevented or easily treated if caught early.
Gastroparesis and diabetes – Gastroparesis is a disorder that affects people with both type 1 and type 2 diabetes. It is a condition in which the stomach takes too long to empty its contents. It causes heartburn, nausea, vomiting, weight loss and other symptoms.
Depression – Feeling down once in a while is normal. But some people feel a sadness that just won’t go away. Life seems hopeless. Feeling this way most of the day for two weeks or more is a sign of serious depression.
Information courtesy of the American Diabetes Association Web site at www.diabetes.org.